Vaccines - The Benefits Far Outweigh the Risks
“It's a dangerous business, Frodo, going out your door.”
— J.R.R. Tolkien, Lord of the Rings
Possibly the most dangerous things out there are so small that 100 million of them could fit on the head of a pin – disease-causing agents.
If you’re alive, you’re subject to attack from these nasty little buggers, which have wreaked havoc throughout history. They have felled mighty armies and wiped out civilizations.
Our most effective and least costly weapon against infectious disease by far is vaccines, which are one of the greatest public health successes ever.
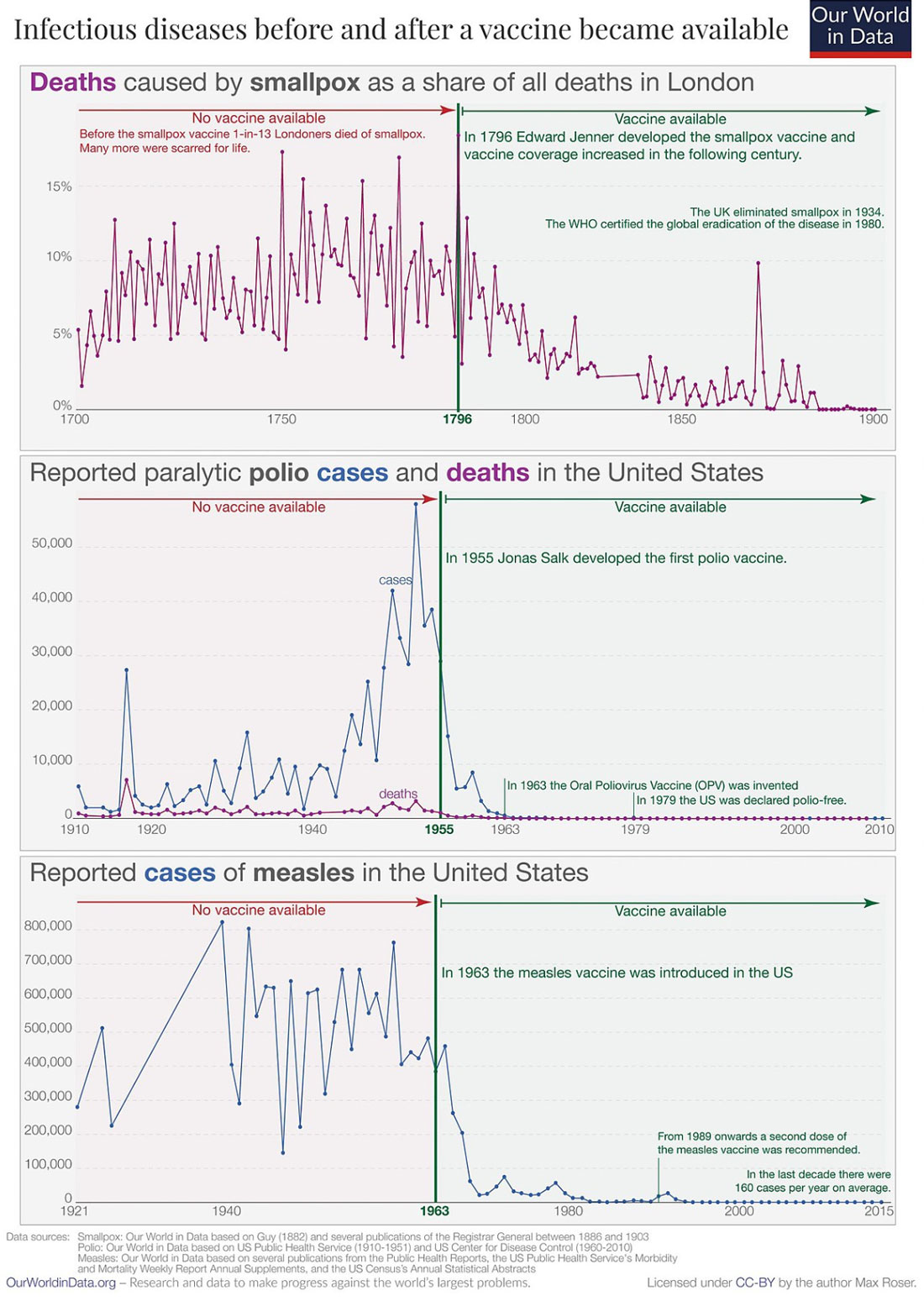
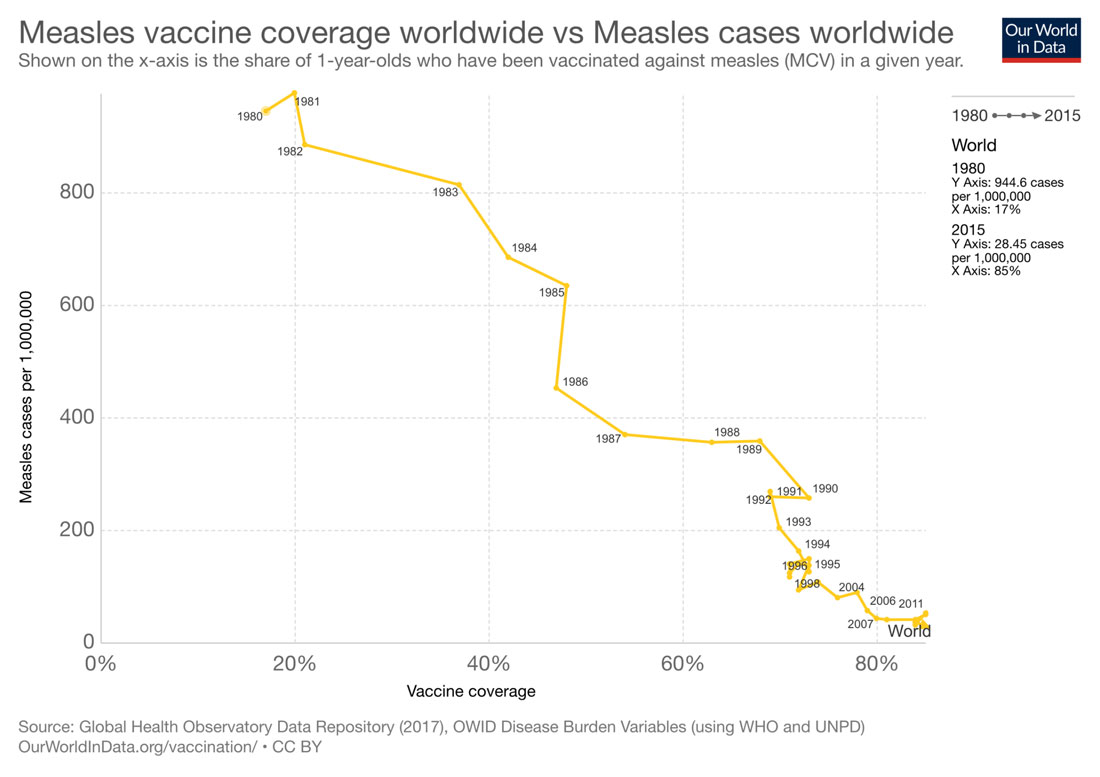
This chart from Our World in Data dramatically illustrates the success of three vaccines - smallpox, polio, and measles - in saving millions of lives.
Immunity
Vaccines act by interacting with your body's natural immune system to help protect you from diseases that once killed millions.
As a multicellular creature, you have dedicated cells or tissues to deal with the threat of infection. Some of these cells kick in immediately to contain an infecting invader. Others respond more slowly but are customized to combat particular invaders. These defensive forces together make up your immune system, which is essential for your survival in a world full of potentially life-threatening microbes.
Your immune system has two levels of immunity against viruses, bacteria and worms, which are called pathogens when they cause disease. Your skin and mucous membranes are your outer protective wall. When pathogens breach these barriers, they can make you very sick.
When these invaders get past your wall, some of your white blood cells fight the invading pathogens and neutralize them. However, these cells are unable to address some infectious threats. That’s when you need specific immunity. White blood cells known as lymphocytes and produced in the bone marrow can mature and differentiate into plasma cells that produce antibodies specifically targeted to a particular threat circulating in the blood. Regulatory cells help control your immune response and recognize when a threat has been contained, then send signals to stop the attack.
The cells that make up a specific immune response both circulate in the blood and are in organs and tissues that make up your immune system, such as the thymus, bone marrow, lymph nodes, spleen, appendix, tonsils, and Peyer’s patches in the small intestine.
If the body responds quickly and effectively to a pathogen, the infection will be eliminated or contained and you won’t get sick. If you develop symptoms, the infection has caused disease. This occurs when your immune system is weak, the pathogen is virulent, and/or the number of pathogens is high.
Vaccines Stimulate Immunity
Vaccination stimulates a specific immune response that creates memory cells specific to a pathogen. These memory cells enable the body to quickly and effectively respond if the body has a future encounter with that pathogen.
Vaccines are just one way in which a person can become immune to a disease. Contracting a disease such as measles also can lead to lifelong immunity. Unborn infants also gain temporary immunity from their mothers’ antibodies and white blood cells, and newborns receive temporary immunity through breast milk. This protection wanes by the time a baby is six months old.
Passive immunity also can be acquired by getting purified blood products from immune people or animals. Passive immunity, unlike vaccines which take weeks or months to produce immunity, can prompt an immune response within hours or days.
It also can help people with weak immune systems whose bodies don’t respond to immunization. One monoclonal or pure antibody produced from a single parent cell is commercially available for RSV in high-risk infants. Physicians also use monoclonal antibodies to fight some cancers, multiple sclerosis, rheumatoid arthritis, Crohn’s disease, and cardiovascular disease.
However, antibodies must be harvested from the blood of hundreds or thousands of human donors or immune animals. In the case of antibodies harvested from animals, the recipient also can have a serious allergic reaction. Many antibody treatments must be administered through intravenous injection, which is complicated and shorter-lived than injecting a vaccine.
This makes vaccines currently the most viable and cost effective way to prevent infectious disease.
How Vaccines Work
The first human vaccines against viruses were based on the idea of using weak viruses to generate immunity without giving the recipient the illness. The smallpox vaccine used cowpox which is similar to smallpox but usually didn’t cause serious illness. The first virus for humans that was weakened in a lab was rabies.
Vaccines can contain these weakened or altered viruses; inactivated or dead organisms or viruses or inactivated toxins or segments of pathogens that trigger the immune system; or just the genetic material.
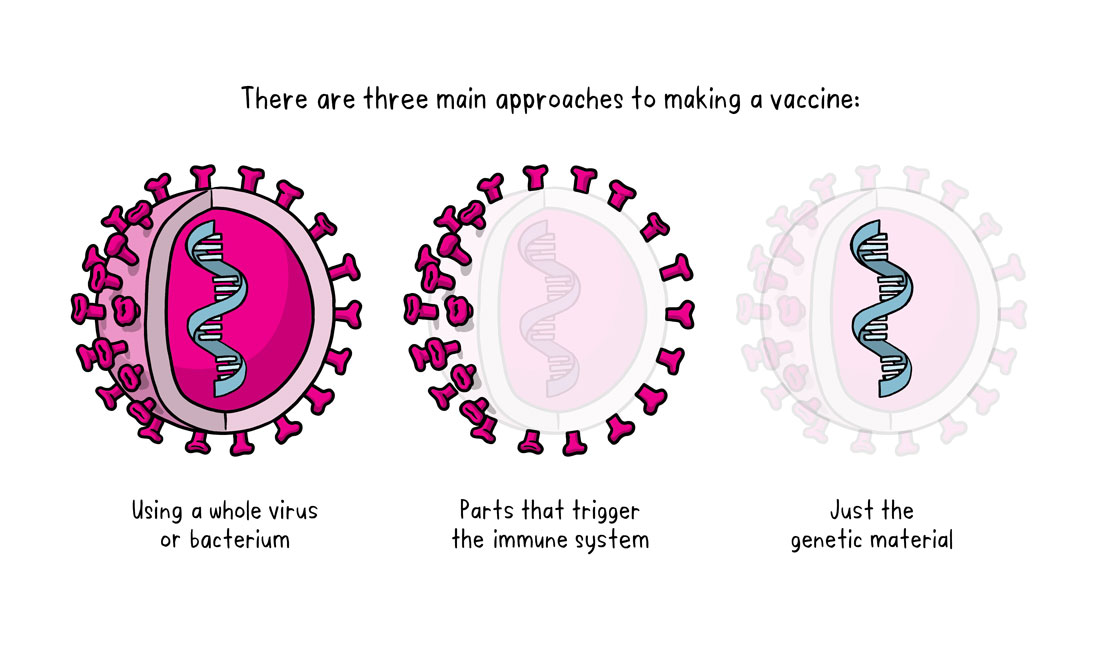
World Health Organization, CC BY-SA 3.0 IGO
Some viruses are passed through cell cultures of animal embryos, typically chick embryos, so that the virus improves at replicating chick cells, but loses the ability to replicate in human cells. The viruses are passed through some 200 embryos or cell cultures until they won’t replicate well or at all in human cells and can be used in a vaccine. When given to a human, the vaccine virus won’t replicate enough to cause illness, but still will provoke an immune response that protects against future infection.
Scientists watch for the unlikely possibility of mutations that could replicate in the body and lead to a more virulent strain. Because the oral polio vaccine can mutate in rare cases and cause paralytic polio, an inactivated polio vaccine is used instead. However, protection from a weakened vaccine typically outlasts protection provided by an inactivated vaccine.
Inactivated vaccines are created by inactivating a pathogen, typically using heat or chemicals that destroy the pathogen’s ability to replicate while allowing the immune system to still recognize it. These vaccines can’t cause disease, but their protection is shorter than that of live vaccines and more likely to require boosters. An example is the seasonal flu vaccine.
Some vaccines use a specific part of a pathogen to provoke an immune response.
Animals have been used in industrial production of vaccines since the late 19th century, either by using animal cells or growing pathogens in live animals. Growing pathogens in live animals is not ideal because the animals are expensive and require extensive monitoring to maintain their health and for research. Some pathogens such as the chickenpox virus don’t grow well in animal cells. When growing viruses in chicken eggs, production can be disrupted if the chickens that produce the eggs get sick with another illness.
This makes the technique of cell culture a significant advance in vaccine production. A cell culture in which cells are grown is taken directly from living tissue. Subcultures are taken from an original primary culture until just one type of cell remains. These are called cell strains. Mutations or manipulations in the laboratory can cause some cell strains to reproduce indefinitely.
Researchers grow human pathogens like viruses in cell strains, weakening the viruses by manipulations such as repeatedly growing them at a lower body temperature. To keep replicating, the virus adapts to growing at the lower temperature and loses its ability to grow well and cause disease at normal body temperatures. When it’s used in a vaccine and injected into a human at normal temperature, the virus will provoke an immune response but can’t replicate enough to cause illness.
Ethical Concerns
This way of producing vaccines in large quantities is one of the most controversial ethical aspects of vaccine development.
In 1936, researchers at the Rockefeller Institute grew poliovirus in a culture of brain tissue from a human embryo. Thirteen years later, researchers at the lab of John Enders at the Children’s Hospital in Boston grew the virus in a culture of skin and muscle tissue from a human embryo.
In 1962 and 1970 respectively, the two main human cell strains used in currently available vaccines – the WI-38 strain and the MRC-5 cell strain - were developed from original cells from aborted fetuses. A large bank of WI-38 and MRC-5 cells was created to serve vaccine production needs.
Common vaccines created using one of these strains are hepititus A, rubella, varicella (chickenpox), shingles, adenovirus, and rabies.
A rubella epidemic caused serious birth defects in the mid-1960s, and some women terminated their pregnancies because they were at serious risk of having children with birth defects. After one abortion, a fetus’s kidney was tested and isolated. At the same time, a cell strain was created using lung cells from another aborted fetus. Many viruses were found to grow well in this cell strain and it was safe to use for human vaccines. After the virus had grown through cells 25 times at a lower temperature, it was no longer able to replicate enough to cause illness in a human, but still provoked a protective immune response. The rubella vaccine developed through this cell strain is still used throughout much of the world as part of the MMR (measles, mumps, and rubella) vaccine. As a result, the Americas have been declared free of the rubella virus.
Anti-abortion and faith groups have raised ethical questions about the human fetus origins of the cell strain. At the same time, researchers have estimated that vaccines made in the cell strain and its derivatives have prevented nearly 11 million deaths and prevented (or treated in the case of rabies) 4.5 billion cases of disease.
This difficult and unresolvable ethical issue has prompted some faith organizations to formulate policies around vaccines. For example, the National Catholic Bioethics Center’s position is that individuals should when possible use vaccines not developed with the use of these human cell strains. However, when the only vaccine available is made from human cell strains, Catholics are free to use it because the risk to public health outweighs the legitimate concern about the vaccine’s origins. This is especially so for parents, who have a moral obligation to protect their children’s life and health and those around them.
The center notes that Catholics should encourage pharmaceutical companies to develop future vaccines without using human cell strains. The center also has pointed out that while cells from fetuses aborted almost 40 years ago were used to begin the cell strains, fetal cells are not active ingredients in current vaccines and the cells used in vaccines never formed a part of a fetus’s body.
Vaccines developed using animal cell strains include vaccines against Japanese encephalitis, rotavirus, polio, and smallpox.
The Ethics of Vaccines Are Complex
In addition to the concerns around the original use of fetal cells to produce cell strains for vaccines, there are ethical debates around many other aspects of vaccine development – informed consent, disparities in access, and mandatory immunizations for school entry.
After the HPV virus for human papillomavirus (HPV), a sexually transmitted disease, was approved in 2006, some state legislatures tried to mandate vaccination for girls ages 11-12. Ethical objections included religious concerns that the vaccine could interfere with abstinence-based messages; fears that the vaccine could force a child to undergo vaccination against her family’s beliefs; and concerns about the fairness of providing a vaccine to one gender.
All 50 states allow vaccination exemptions for certain medical conditions; 48 states allow religious exemptions; and 20 states allow exemptions for philosophical reasons.
However, many studies have found that individuals who exercise religious and/or philosophical exemptions are at significantly greater risk of contracting infections which put themselves and others at risk.
The vaccine test process raises ethical questions about control groups that don’t get the test vaccine, testing the vaccine on children, and helping people with low health literacy understand the implications of consent to be given a vaccine.
In the 1970s, several lawsuits were filed against vaccine manufacturers and healthcare providers by people who thought they had suffered ill effects from the diphtheria, pertussis, tetanus (DPT) vaccine. There was a lack of scientific evidence to support the claims, but damages were awarded anyway. Several vaccine manufacturers stopped production because of concern over liability, and a vaccine shortage resulted.
Congress passed legislation to reduce liability and established a requirement that healthcare providers provide a vaccine information statement describing a disease and the related vaccine’s risks and benefits to everyone getting the vaccine. Healthcare providers also must report certain adverse effects after vaccination. Those injured by vaccines can be compensated on a no-fault basis.
Another major ethical concern is that children from families with low incomes and children without health insurance as well as racial minority adults are less likely than whites to receive preventive care, including vaccinations.
COVID-19 Vaccines
The first COVID-19 vaccines authorized for emergency use in 2020 were based on mRNA technology. This technology uses mRNA enveloped in a lipid (fat) sphere. The vaccine is introduced into the body, where the body’s immune cells reveal the mRNA. The mRNA gives the cell “code” to create a protein similar to the “spike” protein on the coronavirus’ surface. The immune cell releases that protein to other immune cells, triggering an immune response that includes antibody production and activation of specialized cells to find and kill coronaviruses bearing that spike protein and infected host cells.
In early 2021, a third vaccine for the COVID-19 pandemic was authorized for use in the United States that used a simian adenovirus that was hollowed out and the mRNA for coding a coronavirus spike protein put inside. The mRNA is introduced into immune cells after those cells take up the simian adenovirus after recognizing it as a pathogen. The immune cell then creates the spike protein and triggers the ensuing immune response.

A busy COVID-19 vaccination center in Spanish Fork, Utah, during the pandemic. Photo by Forrest Anderson.
Influenza Vaccines
Viruses aren’t alive because they need a host organism to reproduce, but they still can evolve and evade the immune system, replicate themselves, and spread to other hosts. They lose characteristics that make it difficult for them to spread in favor of ones that enable them to spread. This is why new influenza vaccines have to be created each flu season. Scientists try to predict how these common flu viruses will evolve so they can create a vaccine designed to fight them. Sometimes it works, and sometimes the vaccines are less effective.

Photo by Forrest Anderson.
Sometimes two or more types of influenza combine to form a different virus. If it can spread easily, it can cause a pandemic because people have few antibodies against the virus.
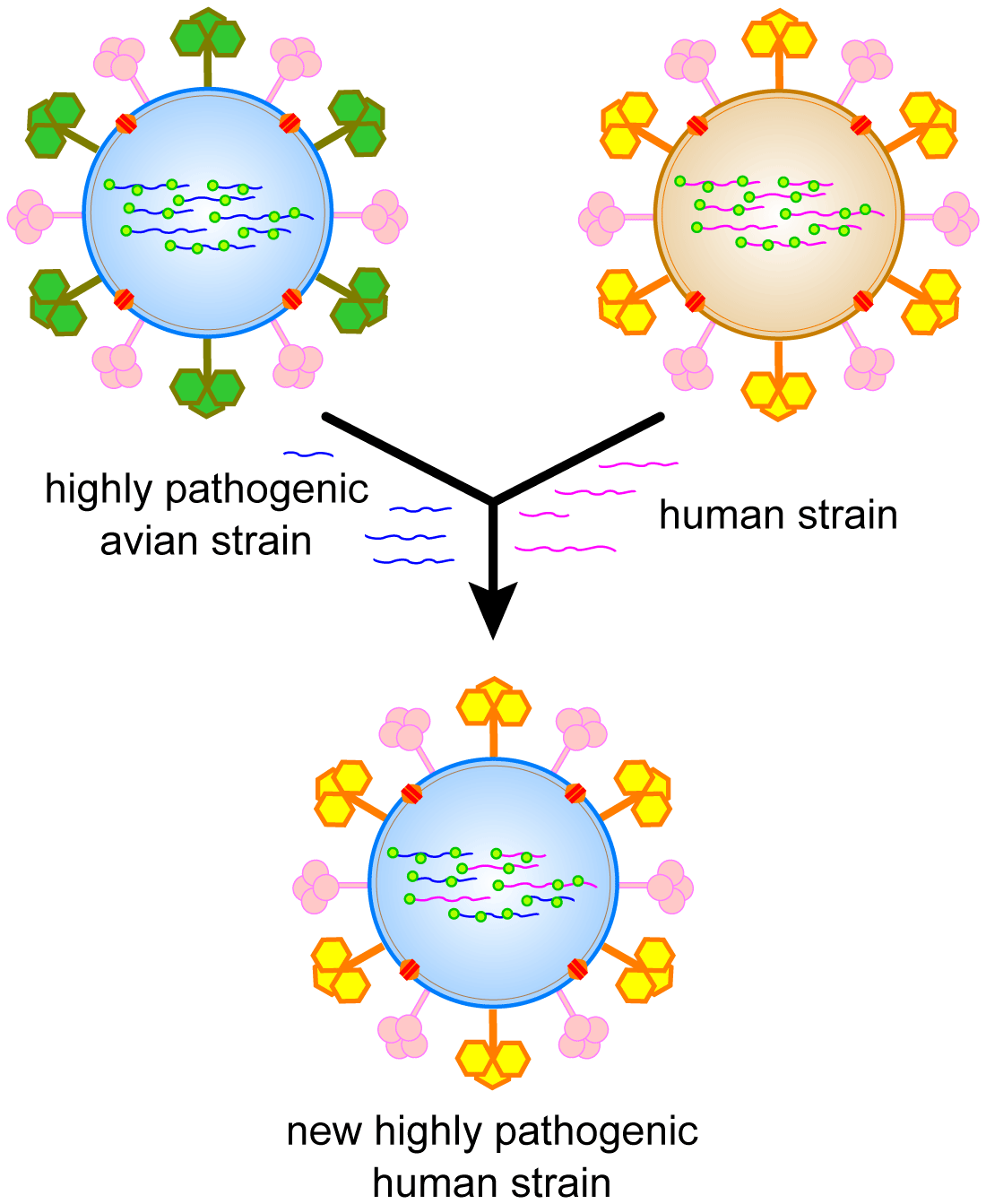
This infographic is available for use under a Creative Commons license.
A pig flu virus and a human flu virus can combine in a bird to create a different flu type that can then spread as the virus jumps from the bird to a human and then mutates in the human.
Can Vaccines Eradicate Infectious Disease?
The only infectious disease considered eradicated is smallpox, which once killed a third of its victims and left others blind or scarred. Other diseases such as rubella are considered eradicated in some countries, but they still cause outbreaks in other places.
The virus that causes Acquired Immune Deficiency Syndrome (AIDS) is highly genetically variable and can create billions of copies of itself daily. When the replication process contains errors, they become genetic mutations that can recombine and form a new virus in a person who has been infected with different HIV variations. As a result, HIV can quickly develop resistance to anti-HIV drugs. It is difficult to create a vaccine for a virus that is rapidly changing.
Yellow fever infects both humans and monkeys through infected mosquito bites, so even if everyone were vaccinated against it, infected monkeys could infect humans whose immunity had waned.
Malaria is difficult to eradicate because getting it doesn’t confer lifelong immunity.
The bottom line is that vaccines can dramatically lower your risk of serious, life-threatening infectious disease, but some of those diseases are unlikely to ever be eradicated.
Government Regulations Around Vaccine Safety and Efficacy
Safety and ethical concerns about vaccines have resulted in a rigorous system for developing, testing, and regulating vaccines in which governments and the private sector cooperate.
Contamination of smallpox and diptheria vaccines in 1901 prompted the passage of the 1902 Biologic Control Act, the first modern federal legislation to control the quality of drugs. The Act established the government’s right to control vaccine making.
The United States Public Service Act of 1944 mandated that the federal government issue licenses for biological products, including vaccines. After a poliovirus vaccine accident in 1954, the Division of Biologics Standards was formed to oversee vaccine safety and regulation. It is the Center for Biologics Evaluation and Research.
Vaccine development in the United States begins with laboratory research to identify antigens that could help prevent or treat a disease. Pre-clinical studies use tissue-culture or cell-culture systems and animal testing to assess the safety and effectiveness of a candidate vaccine. Vaccines are tested on animals to give researchers an idea of the cellular responses they might expect in humans and suggest a safe starting dose for the next phase of research, as well as a safe method of administering the vaccine.

Photo of a virus researcher by James Gathany. This photo is in the public domain.
Researchers vaccinate animals and then try to infect them with the target pathogen. Candidate vaccines that fail to produce the desired immune response are abandoned. When a vaccine is effective in the lab, the sponsoring company applies to the U.S. Food and Drug Administration for approval. Once the application has been approved, the vaccine is tested in three phases.
In phase one, a small group of adults, usually between 20-80, are given the vaccine to assess its safety and determine the type and extent of immune response that it provokes under careful monitoring and controlled conditions. In a few situations, researchers may try to infect participants with the pathogen after the experimental group has been vaccinated.
If the results are promising, several hundred people are given the vaccine in Phase II to study the vaccine’s safety, effectiveness, proposed doses, schedule of administering them, and method of delivery.
If the vaccine is still found to be safe and effective, Phase III larger trials involving thousands to tens of thousands of people are conducted. In this phase, rare side effects can be identified. If this phase is successful, the licensing process is carried out.
The FDA monitors production of licensed vaccines. Optional Phase IV trials may be conducted after a vaccine is released.
The federal government has a Vaccine Adverse Event Reporting System through which anyone can report an adverse event that they think is related to a vaccine. About 30,000 events are reported annually, between 10-15 percent involving serious medical events. Rare adverse events have been found to be related to vaccination.
The Centers for Disease Control keeps the Vaccine Safety Datalink, a collection of linked databases containing information from large medical groups that gather data on vaccination from participating medical groups. It helps monitor new vaccines and possible associations between adverse events and vaccinations.
After Chinese researchers shared the genetic sequence of the COVID-19 virus in early 2020, the U.S. government gave vaccine manufacturers funding to accelerate research on developing a vaccine.
The funding enabled manufacturers to speed up the testing phases, but the three vaccines that were distributed underwent the same safety and efficacy testing as other vaccines do.
Vaccine production and administration involves a variety of U.S. agencies that build national preparedness for pandemics, manage stores of vaccines and drugs to be deployed in national emergencies, and are involved in pandemic and bioterror response.
Military Research
Military researchers have significantly contributed to vaccine development, as infectious disease has historically caused more casualties than bullets in wars.
It felled many American soldiers during the Revolutionary War, prompting George Washington to order mandatory inoculation against smallpox for any soldier who had not previously had the disease. Because smallpox that infected half of American soldiers in the battle of Quebec is believed to have been responsible for the American defeat there, some historians have suggested that if vaccines has been administered earlier, some or all of Canada would now be part of the United States.
Vaccine is One Tool to Fight Infectious Disease
Vaccination works in tandem with quarantine, social distancing, mask wearing and disease treatment during a pandemic such as COVID-19. Partly because it typically takes at least several months to produce the first doses of a new vaccine, social distancing, quarantine, masking, and use of anti-viral medications are used to limit disease spread. Because all of these prevention strategies work together to prevent the spread of disease, the combination of the anti-vaxxing and anti-masking movements were a toxic combination that helped spread COVID-19 and drive up the death toll during the pandemic.
Future Vaccine Research
There is a chronic global shortage of vaccines, so researchers are working on innovations that allow less antigen in each vaccine dose, development of a universal influenza vaccine that might need to be given only once, and plant-produced influenza vaccines. There also is research on better ways to administer vaccines that wouldn’t require a trained medical professional, ways to transport vaccines without cold storage, and ways to make vaccines trigger long lasting responses.
Misconceptions around Vaccines
Common misconceptions:
- That a child’s immune system can be overloaded by receiving multiple vaccines at once. Studies have repeatedly shown that giving vaccines in combination causes no more adverse effects than administering them separately. Delaying vaccines puts children at increased risk of contracting preventable diseases.
- Assuming that because diseases such as polio and measles have disappeared or are rare in the United States, children no longer need to be vaccinated against them. Polio and measles still can infect unprotected people if it is brought into the country.
- That vaccines are ineffective. No vaccination is 100 percent effective, so some vaccinated people with weakened immune systems can contract an infectious illness from an unvaccinated person. During an outbreak, the number of these individuals who get sick can outnumber the unvaccinated people who get sick because few people are unvaccinated. These numbers can cause people to erroneously conclude that the vaccination is ineffective, although 98 percent of those who are vaccinated don’t contract the disease.
- Natural infection provides better protection than vaccine protection. Natural immunity lasts longer in some cases than vaccine-induced immunity, but the risks of dying from natural infection far outweigh the risks of immunization. Some vaccines also provide more effective immunity than natural infections do.
Vaccinations Are By Far The Most Effective Strategy Against Infectious Disease
The evidence is overwhelming in favor of vaccinations as the key strategy to prevent serious and fatal infectious disease. Vaccines have substantially reduced the overall mortality from infectious diseases in much of the developed world. They are one of the greatest success stories in public health. Americans are healthier today because of vaccines than they ever have been and vaccines are safer than ever.
Many of the ethical and professional concerns around vaccines probably never will be entirely resolved, because they are so complex and involve so many moving parts that they defy simple conclusions. However, when measured by the yardstick of realistic tradeoffs, vaccines' record of preventing deaths is overwhelmingly a win.
Is vaccination itself a risk? Sure it is. There are risks of a rare allergic reaction and that a vaccine won’t be effective for the particular microbes that invade your body. However, the risks are astronomically lower and the benefits far higher than taking your chances unprotected from dangerous diseases.
Check out these related items

The Real Cost of COVID
Exit polls showed that many voters saw boosting the economy and controlling the pandemic as competing goals, but experts say they need to happen in tandem.

The Mask of Denial
New studies overwhelmingly show that masks are the most effective way to curb the pandemic and keep the economy working.

What does the future hold?
Dozens of experts’ analysis of long-term trends can help us identify the challenges and opportunities amid the COVID-19 pandemic.